Date: February 2, 2024
Location: Ramada Hotel- Downtown Beyrouth
Prepared by:
Abou Nassar Denise – OST and Shelter Manager , Social Worker.
Akiki Rita- Head Nurse
Germany Jennifer – Psychologist
Opioid Substitution Treatment (AJEM)- Denise Abou Nassar
- Overview
AJEM’s Opioid Substitution Treatment Program (OST) was initiated in 2012 at the Roumieh Center as part of the Harm Reduction Program. Over the years, it expanded to include centers in Rabieh and Chiyah by 2014. However, in November 2020, the Roumieh and Chiyah centers were closed, and all patients are now consolidated at the Rabieh center, where services are available
The primary objective of the OST program is:
- To mitigate the harm associated with drug misuse, particularly the risks of blood-borne infections through needle-sharing.
- It aims to provide substitution treatment for individuals over 18 who are opiate-dependent, have experienced multiple relapses, and struggled to maintain abstinence.
- The OST utilizes prescribed opioid agonists such as Buprenorphine or Suboxone®, which mimic the effects of heroin and morphine on the brain. This helps alleviate withdrawal symptoms, reduce cravings for illicit opiates, and serves as the initial step in stabilizing individuals in crisis.
- Opiate-dependent individuals often face complex challenges related to their medical, psychological, and socioeconomic well-being. To address these issues comprehensively, the program offers multidisciplinary care and support provided by a team of healthcare professionals. The interdisciplinary team consists of a psychiatrist specializing in addiction and substitution treatment, a psychologist, a social worker, and a nurse.
- Collaborating with and operating under the supervision of the Ministry of Public Health in Lebanon, the program ensures that beneficiaries receive treatment and support to maintain good health and achieve psychosocial stability. The holistic approach underscores the importance of addressing not only the physical aspects of addiction but also the underlying psychological and social factors contributing to the individual’s situation.
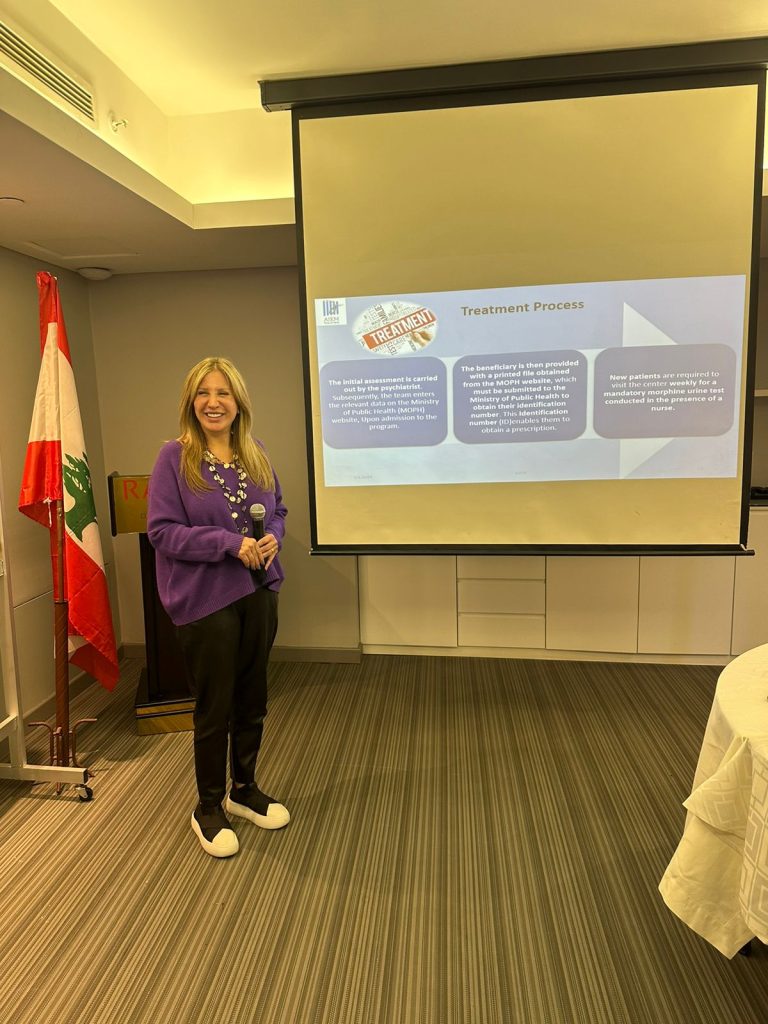
- Treatment Process:
• The initial assessment is carried out by the psychiatrist. Subsequently, the team enters the relevant data on the Ministry of Public Health (MOPH) website, Upon admission to the program
- The beneficiary is then provided with a printed file obtained from the MOPH website, which must be submitted to the Ministry of Public Health to obtain their identification number. This Identification number enables them to obtain a prescription.
- New patients are required to visit the center weekly for a mandatory morphine urine test conducted in the presence of a nurse.
- Following the test, the patient receives a prescription indicating the prescribed medication and dosage from the referring doctor.
- Subsequently, they are instructed to visit a specific hospital pharmacy to purchase the prescribed medication. Each patient must select a hospital upon admission, and they are obligated to obtain the medication exclusively from that chosen hospital.
The prescribed medication is currently available at three public hospitals:
- Rafic Hariri University Hospital (RHUH) in Jnah.
- Daher el Bachek Governmental Hospital (DBGH) in Roumieh.
- Elias El Hrawi Hospital (EHGH) in Zahle.
Eligibility Criteria:
To be eligible for the program, individuals must meet the following criteria:
- Dependent on heroin, Tramadol, or other opiates.
- Age above 18.
- Previous attempts at in-patient detox or rehabilitation.
Exclusion Criteria:
Certain conditions may lead to exclusion from the program. Exclusion criteria may include:
- Severe medical and psychiatric morbidity.
- Prior suspension from AJEM centers.
- Suspension from another non-governmental organization (NGO) due to dangerous or manipulative behaviors, trafficking…
- Other
- Medication:
- The Opioid Substitution Treatment program in Lebanon utilizes two main substitution medications, namely Buprenorphine and Suboxone®.
- In most cases, patients are prescribed Suboxone, with the exception being instances where individuals experience allergic reactions or other adverse medical responses to Suboxone. In such cases, the doctor will opt for Buprenorphine as an alternative.
- Both medications are administered in the form of pills and are meant to be taken sublingually (under the tongue).
- After taking the medication, patients are advised to allow for sublingual absorption and refrain from drinking, eating, or smoking for the subsequent 30 minutes.
- It is crucial to emphasize that the medication should never be injected, as this can pose harm.
- Random check-ups for intravenous (IV) marks are conducted by the nurse to ensure adherence to this guideline.
- Patients are also instructed to abstain from consuming alcohol or taking benzodiazepines, and the rationale for this is clearly stated.
- It’s noteworthy that Suboxone® may gradually replace Buprenorphine due to the latter’s potential harm when injected. Suboxone contains naloxone, a substance that counteracts the medication’s effects if injected, thereby serving as an additional safety measure.
- Top of Form
C. Prescription books:
- Prescription books for the Opioid Substitution Treatment (OST) are obtained from the Ministry of Public Health (MOPH). Each book comprises about 50 blank prescriptions, which must be stamped with the ministry’s logo; otherwise, it cannot be utilized.
- Prescriptions are prepared every week for new patients. When a prescription book is exhausted and no longer contains blank prescriptions, it is necessary to obtain a replacement from the Ministry of Public Health (MOPH).
- Each prescription has a validity period of only 2 days: If the patient fails to purchase the medication within this timeframe, the prescription becomes void. In such cases, the patient needs to reach out to the treatment center for a new urine test and, if feasible, a new prescription.
Prescriptions enable patients to obtain medication for a one-week (7-day) period and are renewed every week at the center after the urine test. - Once patients attain medical stability and exhibit a minimum of 3 months of compliance with treatment conditions, they can shift to a two-week schedule, enabling them to procure medications for a 2-week duration, and in such instances, prescriptions are renewed biweekly.
D. Testing:
- Mandatory morphine urine tests are conducted every week for all patients before issuing a prescription.
- Only patients approved for the 2-week schedule by both the Ministry of Public Health (MOPH) and the prescribing doctor are eligible for testing every two weeks.
- If, for any reason, a patient is unable or chooses not to undergo the test, they will not receive a prescription, consequently preventing them from purchasing medication at the hospital.
- The testing process is overseen by the nurse to prevent any manipulation.
- Additionally, a compulsory buprenorphine urine test is administered once a month for all patients to ensure proper medication adherence. Random urine tests for multiple substances, including cocaine, benzodiazepines, morphine, and THC, can be conducted at the discretion of the prescribing doctor to verify the absence of other substances in the patients’ systems.
E. Discontinuing or stopping the treatment
- Discontinuing the treatment abruptly is discouraged due to the potential onset of withdrawal symptoms.
If a patient intends to cease medication, they should consult with their prescribing doctor beforehand
- Opioids and Naloxone Administration – Rita Akiki
The third part of the workshop focused on opioids, encompassing their definition and medical uses as well as their harmful effects when used illicitly. The discussion also addressed opioid overdose, including its definition and common symptoms. An examination of naloxone as an opioid antagonist was provided, detailing its appropriate administration. The segment concluded with a comprehensive guide to responding to opioid overdoses, outlining five key steps (Shouting and stimulation, calling emergency services, performing rescue breathing and/or chest compressions, administering naloxone, and repeating steps 3 and 4 if necessary.). Participants engaged in a hands-on demonstration of naloxone administration to enhance their understanding.
- Substitution Treatment
The fourth part of the workshop focused on providing in-depth information regarding opioid substitution treatment, specifically comparing methadone and buprenorphine in terms of pharmacology, mode of action, clinical applications, administration methods, half-life duration, and associated risks. Additionally, a protocol for buprenorphine administration was outlined.
- HIV/AIDS
A- Global HIV Statistics – 2023
The workshop presented global HIV statistics for 2023, including an epidemiological analysis revealing a total of 40.4 million people living with HIV until July 2023. The distribution of HIV cases was discussed based on the profiles of individuals living with HIV.
B- National HIV Statistics (in Lebanon) for 2023
The session reviewed the national HIV statistics for 2023 in Lebanon, presenting a cumulative total of 2,731 reported cases up to November 30, 2023, with 261 new cases identified between December 1, 2022, and November 30, 2023. Additionally, the session provided an analysis of HIV/AIDS cases over the past seven years, focusing on various aspects:
– Gender distribution (2023: 88% men, 8% women, and 4% others)
– Distribution by age groups (2023: 0-15: 0%, 15-29: 45%, 30-49: 43%, and >50: 12%)
– Modes of transmission (2023: 88% through sexual intercourse)
– In-depth discussion on distribution based on sexual orientation (2023: 72% homosexual)
C- Understanding HIV/AIDS
This section provided an in-depth understanding of HIV/AIDS, covering its definition, symptoms, modes of transmission, risk factors for transmission, prevention strategies, HIV testing methods for screening and diagnosis, and treatment in Lebanon, including Pre-Exposure Prophylaxis (PrEP) and Post-Exposure Prophylaxis (PEP).
D- Self-Testing
The workshop concluded with a discussion on oral HIV self-testing, including technical information and the distribution of testing kits to participants for their awareness and utilization.
Stigma And Discrimination towards Drug Users and PLHIV( people Living With HIV)- Jennifer Germany
In this workshop, the concepts of stigmatization and discrimination are explored, particularly in the context of substance abuse and HIV. Stigmatization is described as a social process whereby individuals or groups are marked, rejected, or treated differently due to perceived deviant or stigmatizing characteristics. Discrimination, on the other hand, involves treating someone unfairly based on specific attributes such as race, gender, religion, mental health, addiction, or HIV serostatus.
The workshop highlights the stigmatization and discrimination faced by individuals dealing with substance abuse and those living with HIV. This includes negative perceptions related to moral weakness, lack of willpower, or criminality, leading to social, professional, and familial stigmatization. Such challenges can create barriers to treatment and social reintegration.
The profound impacts of stigmatization and discrimination on mental health, relationships, and personal life are discussed, encompassing stress, anxiety, depression, isolation, low self-esteem, suicidal thoughts, self-stigmatization, high-risk behaviors, and obstacles to opportunities. The effects on the immune system and personal life, including reluctance to use naloxone due to hesitation or limited access, are also addressed.
The workshop provides strategies to combat stigmatization and discrimination, including adopting a non-judgmental attitude, using inclusive language, continuous education and training, active listening, promoting accessibility and availability for questions, respecting client autonomy, ensuring confidentiality, creating a welcoming environment, and providing educational resources. Additionally, support for anti-stigma campaigns, participation in community initiatives, leadership sensitive to stigmatization, media education, and collaboration through partnerships are emphasized.
The importance of integrating formal non-discrimination protocols in healthcare settings, with clear guidelines on preventing stigmatization, is underscored. The necessity of welcoming and non-stigmatizing services for substance use disorders, grounded in values like non-discrimination, respect, dignity, compassion, judgment-free approaches, person-centered practices, strengths-based approaches, holistic care, accessibility, flexibility, and responsiveness is emphasized. The workshop concludes by urging collaboration with organizations and others to implement comprehensive strategies collectively. In order to counteract stigma and discrimination, the collaborative efforts of a multidisciplinary team are directed towards achieving success.